“Our research opens up a whole new approach – the vaccine approach – to effective treatment of melanoma, even in the advanced stages of the disease,” said Tel Aviv University Prof. Ronit Satchi-Fainaro.
By Aryeh Savir, TPS
Researchers at Tel Aviv University have developed a nanoparticle that can be used to vaccinate against melanoma skin cancer, Tel Aviv University announced Monday.
Led by Professor Ronit Satchi-Fainaro, head of the Department of Physiology and Pharmacology and head of the Cancer and Nanomedicology Laboratory of the Faculty of Medicine at Tel Aviv University, the team developed a vaccine that has shown to be most effective in model mice in three primary situations: as a prophylactic treatment, as a drug for treating primary tumors, and for the eradication of metastatic cancer.
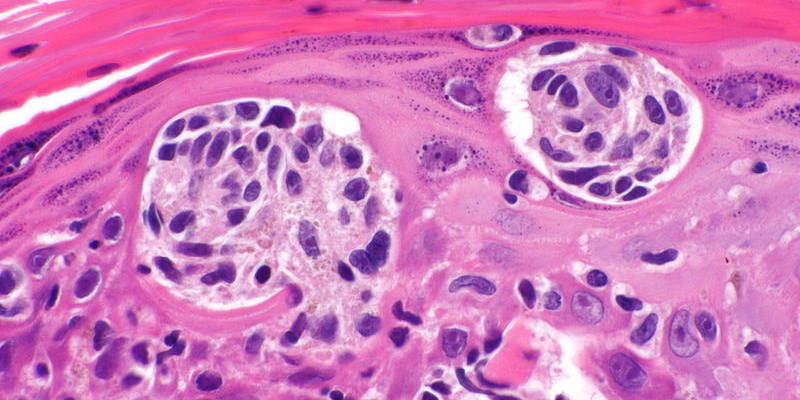
The researchers developed tiny particles made of a biodegradable polymer, about 170 nanometers in size. Within each particle, they “packed” two peptides, short chains of amino acids, which are characteristic of melanoma cells. They then injected the nanoparticles into model mice contending with melanoma.
“These nanoparticles carry on their back a sugar molecule that serves as an ‘arrowhead’ that targets immune system dendritic cells that activate T cells, which in turn attack the tumor,” Satchi-Fainaro explained.
“These particles worked just like the known virus vaccines: they stimulated the mice’s immune system when the immune cells learned to identify and attack cells containing the two ‘packaged’ peptides – that is, the melanoma cells. This means that the vaccinated mouse’s immune system will now attack the melanoma cells, if and when they appear in the body,” she said.
Later in the study, the researchers examined the effectiveness of the vaccine in three different situations.
First, as a preventive measure, the vaccine was injected into healthy mice, and then melanoma cells were injected. The result was that the mice did not get sick, which means the vaccine prevented the disease.
Second, the vaccine was tested as a therapy for a primary tumor. A combination of the new vaccine and immunotherapy treatments was tested on model mice with melanoma. The combined synergistic treatment significantly delayed the progression of the disease and greatly extended the lives of all treated mice.
In the third case, in the treatment of metastatic cancer, the researchers examined human tissues of brain melanoma metastases removed from patients. Brain metastasis is a major cause of mortality in patients who were diagnosed late. The research found that the sick tissue contained peptides and was a target for the vaccination.
“The war on cancer in general and melanoma in particular has been evolving over the years through a variety of therapeutic methods such as surgery, chemotherapy, radiation and immunotherapy. But the vaccine approach, which has proven so effective against various viral diseases, has not materialized yet against cancer, Satchi-Fainaro said.
“In our study, we have shown that it is possible to produce an effective nano-vaccine against melanoma and to sensitize the immune system to immunotherapies.
“Our research opens up a whole new approach – the vaccine approach – to effective treatment of melanoma, even in the advanced stages of the disease,” she added. “We believe the method we have developed may also be compatible with other types of cancer, and we believe our work is a solid foundation for the future development of human cancer vaccines.”