Eliana Steinberg is the driving force behind a tiny chip that tests several treatments on the same tumor in record time, and she’s only 28.
By Roni Dori, CTech
Eliana Steinberg was a pharmacist in a pharmacy in Jerusalem when she encountered a patient who changed her life.
“He had prostate cancer in an advanced stage with metastases, and he would come to the pharmacy several times a month. I developed personal relationships with him and his wife,” she tells Calcalist.
“It was really sad to see before my eyes the progress of his illness and his helplessness, especially when he was facing difficult treatments, which he was not at all sure would be successful. I wanted to help him practically with the disease itself, beyond giving explanations on how to take the medicines. I wanted to ease his suffering.”
Steinberg decided to apply for a master’s degree in a track for excellence in nanotechnology at the School of Pharmacy of the Hebrew University.
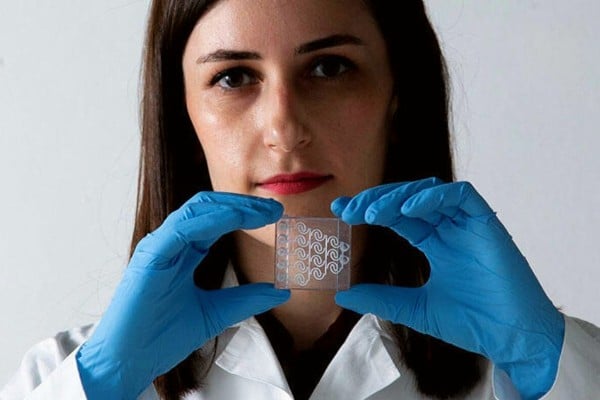
Since then, her studies have developed into a doctorate, and in the last four years Steinberg has developed a method that may cause a huge revolution in the way cancer patients are treated: a transparent chip, which with the help of a tiny sample from a cancer tumor examines a series of possible treatments to see which of them is the most effective, and in record time, with the results obtained in less than two weeks.
“Nowadays, it is possible to know if patients are responding to a certain treatment only after a few weeks or months,” explains Steinberg.
“It is sad because for some of them, by the time they reach this stage, there is no time left to try other treatments, and they miss the opportunity to receive the treatment that was right for them. Furthermore, while they develop metastases, their bodies are further weakened by the chemotherapy treatments, and their ability to cope with the next treatment decreases. My method is designed to bypass this limitation.”
The development, which was done under the direction of Prof. Ofra Benny, is already being used by oncology patients from the Hadassah Hospital under the approval of the Helsinki Committee, which approves experiments on humans. In the coming year, a commercial company will be established on the basis of the development, even before it enters the regulatory approval process.
Meanwhile, the chip earned Steinberg the prestigious Adams scholarship of 100,000 shekels which she received last week.
“We are talking about hundreds of treatments that can be tested in a relatively short time,” explains Prof. Moshe Oren, a biochemist and cancer researcher at the Weizmann Institute and chairman of the steering and selection committee of the scholarship program, which is shared with the Israel Academy of Sciences and Humanities and the Canadian Adams family.
“Once the effectiveness of Eliana’s development is proven, undoubtedly it will have a far-reaching effect for cancer patients,” Prof. Oren said
How the Chip Works
How is the “tumor on a chip” model developed by Steinberg work?
A piece of tissue a few millimeters in size is taken from the tumor, and broken down in the laboratory into hundreds of individual cells. Using the 3D petri dish technique, hundreds of “models” of the original tissue are rebuilt from these cells, which contain all of its cells – cancer and surrounding tissue.
The hundreds of regenerated tissues (called “spheroids”) are then inserted into a chip inside of which are several channels, in each of which a different drug is delivered to the tissues. After about a week, the results of the various treatments are examined and it is concluded which one is the most effective against the tumor.
The model developed by Steinberg belongs to the branch of microfluidics – a field of research that combines engineering, physics, chemistry, microtechnology and biotechnology, and deals with the behavior, and control, of liquids in tiny dimensions, the size of microns.
For example, NASA uses a “lab on a chip” – a silicon chip that contains miniature test tubes and monitoring sensors, into which experimental materials such as cultures, bacteria and chemicals are directed – among other things to scan DNA and organic molecules in search of signs of life in space.
“Organ on a chip” – a chip in which tissues of various organs grow – is another step in the evolution of the field, which combines the advantages of experiments in a test tube (in vitro) with experiments in animals (in vivo): on the one hand, there is an experiment on living tissue without harming animals in a process that may take a long time and end in failure, and on the other hand, the laboratory conditions allow unlimited experiments without harming the patients.
The hope is that in the future this technology will replace laboratory animals in drug development and toxin testing processes.
“One of the things I like most about my research is that it is very clinical, it’s not that I’m researching something abstract and maybe later it will be something applicable, it’s really practical – you come and see the results in the clinic,” says Steinberg. “The ideal for me is that my chip will become something accessible to the public as part of the cancer treatment routine.”
‘If a Door is Closed to Her, She Enters Through the Window’
The most surprising thing about Steinberg’s resume is her age – only 28 years old. “There are people who begin their doctorates long after the age of 30, and there are those who run, like Eliana,” Prof. Oren says of her. Steinberg qualifies it with a smile that “I’m only considered a little bit younger in the lab, and not in an extreme way.”
She was born in a religious family, the daughter of a couple who immigrated from the United States, the youngest of six brothers and sisters. She grew up in Jerusalem and still lives there today. After completing her national service, where she helped students with learning difficulties and new immigrants, she studied for a bachelor’s degree in pharmacy at the Hebrew University, graduating with honors.
“It is important to me that my work be meaningful, and that I can see how I help people directly. I wanted to combine the theory with the practical,” she says. “Being a pharmacist is like having boots on the ground, I felt that I really see the patients and their needs and connect with them on a personal level. It made me want to help them even more.”
So why didn’t you study medicine?
“I was less looking for direct contact with patients, and more interested in developing treatments. Pharmacy seemed to me an interesting and important profession with work.”
What was it about that patient from the pharmacy that pushed you to switch to research?
“Beyond the personal connection, that patient had a cancer of a type that is considered to be one that can be dealt with, and not of the fatal type where there is no chance of helping him. Therefore, I was sad to see him in his condition, knowing that all of this would have been avoided if he had been diagnosed earlier, and not at an advanced stage with metastases. I felt helpless that I had no way to help him.”
How does a pharmacist come to develop chips in cancer research?
“It is indeed a non-trivial transition,” explains Prof. Benny, head of the nanomedicine laboratory at the School of Pharmacy in the Faculty of Medicine at the Hebrew University and Steinberg’s supervisor. “Eliana is on an excellence track in nanotechnology, one of whose strengths is that it exposes the students to a great many disciplines related to materials and engineering.”
Says Prof. Benny, “But her case is much more than that – this is a determined and creative person. If something doesn’t work, she will find a way to make it work. If a door is closed to her, she enters through the window. This is something that not every student knows how to do. And she merges the good and important foundation of pharmacy with the engineering field and the knowledge of 3D graphic design that she acquired. The sky’s the limit for her.”
Steinberg joined Benny’s lab in October 2018, about a year after the lab began developing an organ on a chip, and contributed to a significant boost to the research. “My technology makes it possible to adjust the size of the chip exactly to the amount of tissue I want to test, and to the amount of chemotherapy I need to test in different combinations and concentrations,” she explains, “it’s a very convenient method that is adjusted exactly to each experiment.”
The method of creating the spheroids – those reconstructed tissues that are produced in the laboratory from each cancer cell sampled from the patient – is also not self-evident.
“The spheroids, which are usually formed within one day, can be produced inside the chip or inserted into the chip from the outside,” Benny explains. “The structure of the chip we developed and the materials make the cancer cells prefer to stick to each other instead of spreading on a surface, so they autonomously produce a three-dimensional spherical structure, instead of the structure of cells on a surface that is common in experiments.”
Benny stresses, “This is a critical difference, because in the spherical structure they begin to behave similarly to how cancer cells behave in the body in terms of metabolism, oxidation and more.”
Steinberg’s chip had to overcome some significant technical hurdles along the way. “There was concern that the chip would be toxic to the cells, because it is made of plastic and may secrete substances toxic to the cells, so my protocol makes the substances non-toxic,” explains Steinberg.
“Additionally, we had to make sure that the chip was transparent so that it could be photographed under a microscope, find a way to open and easily remove the tumor from the chip without any leaks, and allow the cells to be grown for a period of time inside it. Finally, I was able to develop a technology that enables all these features and also print the chip in a 3D printer quickly, within two hours.”
How does a pharmacist know how to design a chip that is printed in a 3D printer?
“I studied on my own. There was no design course in my studies, so another doctoral student in the laboratory, who specializes in 3D printing, introduced me to this world. I feel that I have really been fortunate because I enjoy design, love creative thinking, the challenge of overcoming the limitations of the printer and the chip, and the challenge with everything needed to achieve the goal. Since the chip is customized, I have to think of a different design each time according to the needs of the research.”
You make it sound simple, but it’s really complex for someone who doesn’t come from the engineering field.
“For someone who comes from engineering, it’s easier just in terms of knowing how to use the software – it’s something that took me hours at first. But that engineer still lacked the background in biology and especially the understanding of what the living tissue needs. So, in any case, the development of the chip requires a look at both worlds, both engineering and biology.”
From the Pharmacy to Outer Space
Despite its research acceleration, the field of “organ on a chip” is still only at the beginning of its commercial journey: there are several companies in the market (primarily the Dutch Mimetas and the Spanish Beonchip, alongside the Israeli Tissue Dynamics of Prof. Jacob Nachmias).
“One of the disadvantages of the competing technologies is that they require a sample of quite a lot of material from the patient’s tumor,” Benny explains.
“With our method, we maximize the area, which means we are able to use a very small amount of tissue in a very efficient way, and we can try a maximum of drugs on this small amount. We also have the advantage of dynamic analysis, which means we are able to look at tissues and analyze them at different points in time, and this has a great significance in examining how the patient reacts to the drugs. We can also play with the designs according to the research need – printing in the laboratory allows us to control geometric shapes, which others have not been able to do with the standard methods.”
You are describing a breakthrough here.
“This is definitely a technological breakthrough, which could be a game changer in the field. It is a crowded field, and there is a lot of ‘organ on a chip’ research, but we have many unique advantages, so we are definitely optimistic that our development will give a boost to the field of drug prediction.”
The revolutionary chips are now in the validation phase, having so far examined about 30 tumors of oncology patients from Hadassah Hospital. “We constantly continue to perfect the system and make it even more sophisticated,” says Steinberg.
What else needs to be improved?
“Mainly to make the chip even faster, i.e. to reduce it from two weeks to one week. For that you have to go into electrochemistry and adjust the model so that it has as many accurate indicators as possible from all kinds of directions.”
The patients that Steinberg works with at this stage are cancer patients in advanced stages, those whose chances of survival are low. Therefore, her experiments are currently mainly testing the ability to contain or slow down the growth.
One of these patients was an 8-year-old boy. “It is difficult to separate the pure scientific part from the emotions in such a case,” she says. “I received tumor tissue from glioblastoma, the most violent and aggressive cancer of the brain, which developed in him. So the doctors are trying to do everything possible, and sent samples from the tumor to different laboratories, including ours. And while they were still waiting to hear results from the other laboratories, we were already able to grow the cells and also identify which treatments they responded to and what they were resistant to.”
In another case, an examination of spheroids developed from a patient’s glioblastoma sample identified a mutation in 70% of them, which was not detected in the original tumor at all.
“It’s not that the original tumor didn’t have the mutation at all, because it doesn’t suddenly form within 20 days,” explained Dr. Shai Rosenberg, a neuro-oncology researcher at Hadassah Ein Kerem Hospital.
“It was simply in a negligible minority of the tumor cells and the technology helped diagnose it. Accordingly, we recommended a drug that treats this mutation and works wonders. Although the patient was already in a late stage of the disease and lived only two more months, we were able to give her some relief.” Steinberg and Rosenberg presented the case at the Society for Neuro-Oncology conference, the world’s most important scientific conference in the field of brain tumors.
It’s a huge responsibility on your shoulders — to determine what can save a terminally ill patient.
“I definitely feel the weight of the responsibility,” says Steinberg. “And sometimes I’m even a little afraid to hear the answer from the doctors whether we succeeded or not. The concern for the person behind the experiment is constantly present. I was very happy that we were able to somehow help that patient. It’s very meaningful to me.”
Last December, Steinberg’s chips even reached outer space: spheroids she developed in the laboratory for the International Space Station were launched as part of a SpacePharma project to test the effect of the drug Doxil on cancer cells in zero gravity conditions.
“Space medicine is a young and really interesting field of research,” says Steinberg. “The general idea is that in light of the ever-increasing human intervention in space and the trend of space tourism, it is inevitable that eventually there will also be cancer in space, so we want to examine how all these processes happen in microgravity – if they affect the course of the disease and its treatment.”
You started in pharmacy and went all the way to space. That’s very impressive for a 28-year-old.
“With all due respect to all the interesting and challenging things I went through in the process, in the end my goal has always been to help people. I’m really looking forward to our chip being in the public domain. It will be amazing.”